Looking for some help about your wellbeing? Or maybe you are feeling unwell and are looking for the best option for you. Maybe you’re trying to get healthier to improve your overall health.
Leeds Student Medical Practice are here to help you feel your best, whatever that means for you. This page contains advice and guidance for various topics, if you don’t find what you’re looking for contact us and we’ll try to support where we can.
At Leeds Student Medical Practice, our primary goal is to provide you with the highest standard of care, ensuring that every aspect of your health is addressed with honesty and clarity. Part of this commitment involves using accurate medical terminology when discussing your health.
We understand that certain terms, like “obese” or “morbidly obese,” may be upsetting or uncomfortable to hear. However, these terms are clinical descriptors that help us communicate specific health risks and conditions. Using precise language allows us to assess your health more effectively, guide treatment decisions, and work together on developing a plan to improve your well-being.
Please know that our intention is never to cause distress, but rather to empower you with the information necessary to make informed decisions about your health. We are here to support you and to discuss any concerns you may have about the language we use. Together, we can focus on improving your health in a respectful and constructive way.
Thank you for trusting us with your care.
If you are unwell
There are many different options to you if you’re feeling ill, it’s always good to think about what the best path to getting better is in your situation.
Urgent Treatment Centres
Urgent Treatment Centres can help people who need to see a healthcare professional urgently, but who are not in a life-threatening condition.
We have two centres in Leeds: one in the St Georges Centre in Middleton and one at Wharfedale General Hospital. They are both open every day from 8am until 11pm (including bank holidays such as Christmas Day). You can walk into an urgent treatment centre, or you can call NHS111 or the centre directly.
The centre’s receptionist may not be able to answer the phone because they may be helping patients at the desk.
The Urgent Treatment Centres cannot treat people who have a head injury if they are aged under two years old or over 65. In addition, they cannot treat people with pregnancy related health conditions or babies under 6 weeks old. More details of each centre are below.
ST GEORGE’S URGENT TREATMENT CENTRE
Address: St George’s Road, Middleton, Leeds, LS10 4UZ
Opening Times: 7 days a week including Bank Holidays: 08:00 to 23:00.
If you would like to check how busy we are before you attend, please call 0330 311 5106. Our receptionist will be able to advise if there is a wait or discuss alternative options with you. Please note, the receptionist may be helping patients at the desk and may not be able to answer the phone immediately.
Please note, our services may reach capacity due to queues in our waiting room and/or queues on our triage list. Our receptionist may need to advise you of alternative options if the UTC staff are not able to deal with your illness/injury on the day.
To ensure your health need is dealt with promptly and in the right place please call NHS111 first.
The Urgent Treatment Centre (UTC) will see patients with urgent illness (except babies under 6 weeks old or patients with pregnancy related conditions) which cannot wait for you to see your own GP. The service also supports patients with minor injuries including cuts, bites, sprains, bone, muscle or joint injuries.
Please note that the X-Ray facilities are available until 20:30 depending on the nature of the injury. We are able to X-Ray arms, legs, fingers and toes. We cannot X-Ray facial bones, head, neck, back, chest, ribs, hips, thighs or the pelvis. One of our healthcare professionals will advise you if an x-ray is required.
WHARFEDALE URGENT TREATMENT CENTRE
Address: Newell Carr Road, Otley, Leeds, LS21 2LY
Opening Times: 7 days a week including Bank Holidays: 08:00 to 23:00.
If you would like to check how busy we are before you attend, please call 0113 3921647. Our receptionist will be able to advise if there is a wait or discuss alternative options with you. Please note, the receptionist may be helping patients at the desk and may not be able to answer the phone immediately.
Please note, our services may reach capacity due to queues in our waiting room and/or queues on our triage list. Our receptionist may need to advise you of alternative options if the UTC staff are not able to deal with your illness/injury on the day.
To ensure your health need is dealt with promptly and in the right place please call NHS111 first.
The Urgent Treatment Centre (UTC) will see patients with urgent illness (except babies under 6 weeks old or patients with pregnancy related conditions) which cannot wait for you to see your own GP. The service also supports patients with minor injuries including cuts, bites, sprains, bone, muscle or joint injuries.
Please note that the X-Ray facilities are available until 22:30 depending on the nature of the injury. We are able to X-Ray arms, legs, fingers and toes. We cannot X-Ray facial bones, head, neck, back, chest, ribs, hips, thighs or the pelvis. One of our healthcare professionals will advise you if an x-ray is required.
Pharmacy
If you’re struggling with a minor illness, your local pharmacist may be the best option. Pharmacists can advise on a number of health issues, recommending the best course of treatment.
There are a huge number of resources on the NHS website on hundreds of conditions that provide
advice and guidance. If you know the name of your condition, it’s a great place to start.
Domestic Violence
Experiencing domestic abuse can be frightening and isolating, but you are not alone, and support is available. As a GP practice, our team is committed to offering sensitive, non-judgemental support and guidance. If you or someone you know needs help, please reach out to us. We can arrange urgent appointments, support referrals, and referrals to specialist services.
The Domestic Violence Lead for Leeds Student Medical Practice is Dr Ben Ditchfield
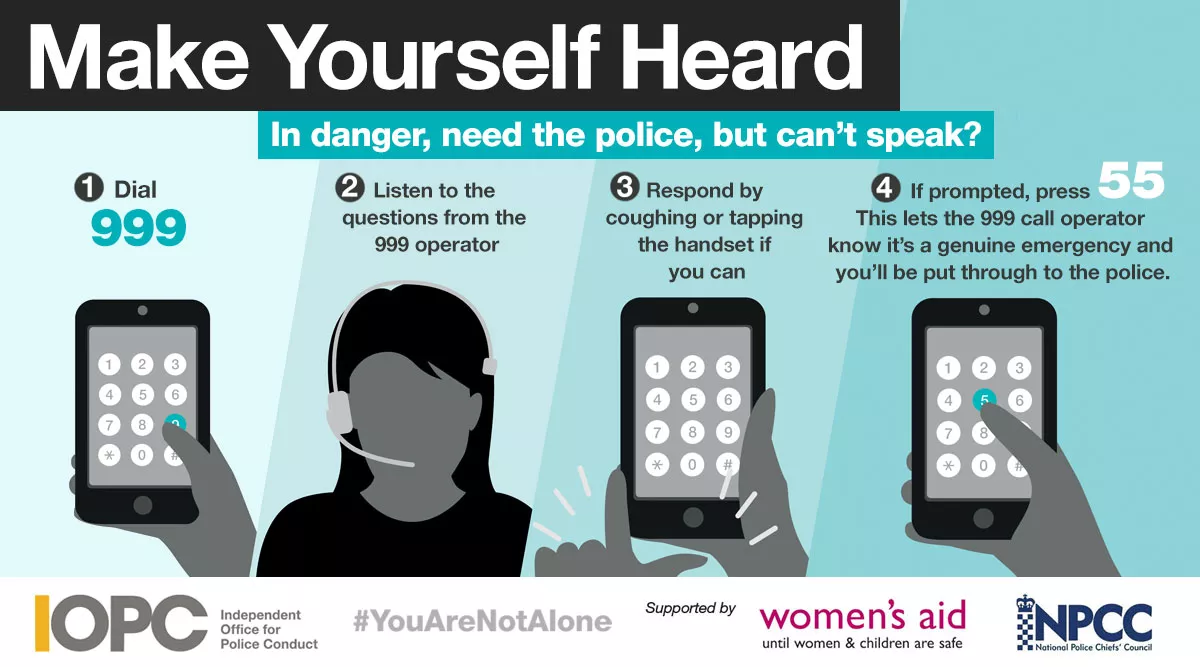
Silent Solutions Police
In an emergency call 999 for the police. If you cannot safely speak to the operator to ask for the Police, stay on the line and the call will be forwarded to an operating system. Press 55 to be transferred to the local police force as an emergency.
Leeds Domestic Violence Service (LDVS)
Support for people of all genders over the age of 16 that have been affected by domestic violence and/or abuse.
24 hour helpline: 0113 246 0401
Email: hello@ldvs.uk
Website: https://ldvs.uk/
Behind Closed Doors
Leeds based support for all genders.
Behind Closed Doors are there at the point of crisis and stay on to work with individuals and families through their recovery. They also deliver preventative activities in the form of training with services, charities, in the workplace and in educational settings.
Website: https://behind-closed-doors.org.uk/
GALOP
Galop gives advice and support to people who have experienced biphobia, homophobia, transphobia, sexual violence or domestic abuse.
Galop operates the National Helpline for LGBT+ Victims and Survivors of Abuse and Violence.
Telephone: 0800 999 5428
Website: https://www.galop.org.uk/
Men’s Advice Line
Men’s Advice Line is a team of friendly Advisors who will listen and believe you, and offer you non-judgmental support, practical advice and information.
Their focus is to increase the safety of men including those who identify as trans, who are experiencing domestic abuse (and the safety of any children) by providing confidential support.
Telephone (Monday–Friday 10am-5pm): 0808 801 0327
Website: https://mensadviceline.org.uk/
Leeds Women’s Aid
Domestic Violence and Abuse Services for women in Leeds.
They can help with legal support, emergency refuge, community and group support, as well as emotional support and advice.
A drop in service is available Tuesday – Friday, for information on where these are held, please call the number below- this is in partnership with LDVS.
Telephone (24hours): 0113 246 0401
Website: Leeds Women’s Aid
An online chat is available Monday to Friday, 1pm to 4pm.
Karma Nirvana
If you are experiencing Honour Based Abuse or facing a forced marriage, Karma Nirvana can help.
Telephone (M-F 9am to 5pm): 0800 599 9247
Website: https://karmanirvana.org.uk/
SignHealth
SignHealth are a charity who help to improve the health and wellbeing of Deaf people.
They run a Domestic Abuse Support service for Deaf People.
Text (M to F 9:30AM to 4:30PM): 07800 003421
Email: da@signhealth.org.uk
If you are struggling with your mental health
If you’re feeling stressed, anxious or depressed, or just want to feel happier, we’re here to help.
If you are LGBTQIA+
At Leeds Student Medical Practice we strive to provide a supportive and safe environment for Lesbian, Gay, Bisexual and Transgender (LGBTQIA+) students. We believe in fairness, equality, and above all value diversity.
While most health issues affecting LGBTQIA+ individuals are similar to those of the general population, we know that LGBTQIA+ people have unique health needs and experience disparities in care.
Below are some key resources that we feel may be of use, but we are happy for you to discuss any concerns with one of our clinical team.
LGBT Foundation is a national charity delivering advice, support and information services to lesbian, gay, bisexual and trans (LGBTQIA+) communities. For more information please click here.
If you want to be healthier
There are many factors that influence a healthy lifestyle, it can be hard to work out what your priorities should be.
Thankfully, there are plenty of resources out there to help support your journey to living healthier and feeling better.
The NHS provide a number of resources that are a good starting point to a healthier lifestyle.
The NHS Live Well page provides a wide variety of information that are a fantastic starting point to a healthier lifestyle.
Closer to home, there are a number of resources on health, food, and smoking cessation among others on the OneYou Leeds website.
If you feel you need additional support, please contact the practice.
If you are planning a family
Whatever you want to know about getting pregnant, being pregnant or caring for your new baby, you should find it here.
If you are travelling
This section is intended to provide guidance for planning your foreign travel from a health perspective. It is more relevant to students taking extended travel breaks, and going to remote areas, than those taking package holidays. The information contained on the separate pages and the links to other web sites should be regarded as a guideline rather than a definitive statement, as the area of travel medicine is constantly changing
With careful planning before you travel, vigilance during and afterwards, you should be able to deal with most medical needs with minimal disruption. Above all else your travel experience should be a fulfilling and enjoyable experience so that you return to Leeds with positive memories and nothing you wish you’d left behind!
Please be aware that practice cannot provide medical advice/issue prescriptions during your time outside of the United Kingdom.
It is important to ensure that you have the required travel insurance in place and if you are unwell/run out of medication while you are abroad, you should seek advice from a local medical service. If you require further advice from the practice, please contact the Reception Team on 0113 295 4488
View the individual sections below for detailed information.
Before you leave
Immunisation and anti-malarials
Make sure you plan your travel vaccinations well in advance, you will often need to start receiving immunisations at least 8 weeks before you leave Leeds.
Before you leave
Immunisation and anti-malarials
Make sure you plan your travel vaccinations well in advance, you will often need to start receiving immunisations at least 8 weeks before you leave Leeds.
Keeping Healthy Abroad
We recommend that you spend some time planning your trip and understanding the health risks you may face during your travels
You can find very useful information on a variety of travel topics at the Government web site Fit For Travel
Sexual Health
Remember that unprotected sex can result in anything from Chlamydia to HIV to unwanted pregnancy. The Sun newspaper reported in July 2005 that a Syphilis outbreak in Manchester was quickly replicated in Amsterdam, Dublin, and Paris as a result of people jetting from place to place and having unprotected sex – everyone going on holiday should take condoms, don’t leave it to chance, it’s not worth the risk.
Rabies
Rabies is present in many parts of the world. If a person develops rabies death is 100% certain. There are 40,000 deaths worldwide every year from Rabies. Do not be complacent – do not touch any animal, particularly; dogs, cats, monkeys, bats. If you are travelling to remote areas, it is particularly important that you consider getting vaccinated against rabies before you travel.
What to do if you are scratched or bitten by a mammal in another country where rabies is present
– Vigorously clean wound with soap and running water for 10 minutes
– Encourage the wound to bleed a little
– Apply tincture of aqueous iodine solution if you have any, or 40% alcohol or stronger (e.g. Whisky)
– Obtain information about the animal concerned
– SEEK MEDICAL HELP IMMEDIATELY (AT THE LATEST WITHIN 24 HOURS OF INJURY). If you have not been vaccinated you will probably require 5 injections plus an injection of rabies immunoglobulin. If you have been vaccinated you may still require 2 further injections within 48 hours
– Do not allow the wound to be stitched unless absolutely necessary
– It is vital that you complete the appropriate course of post-exposure treatment offered
– Please report the incident back to your GP on your return to the UK
An article in the British Medical Journal in September 2005 reported the case of a British woman who travelled to India. Whilst there a puppy bit her, leaving a slight graze. She had not been vaccinated against Rabies, but thought nothing more about it and did not seek medical help. Three and a half months after returning to the UK she was admitted to hospital with severe shooting pains in her lower back and left leg. She was diagnosed with rabies and died after eighteen days in hospital
Schistosomiasis (Bilharzia)
Prevalence: Africa (90% of cases), some parts of Latin America and South-East Asia
If swimming in fresh water lakes and rivers in Africa, Latin America and South-East Asia you are at risk of contracting schistosomiasis. Common hotspots are Lake Malawi (Malawi) and Lake Victoria (Uganda) The best advice is to avoid swimming in freshwater lakes or rivers, or if you do, check the risk of schistosomiasis in that area. In addition it is wise never to go barefoot, but to wear protective footwearwhen out, even on the beach. Other diseases and parasites can be caught from sand and soil, particularly wet soil
If you are exposed to risk, you need a blood test at least 12 weeks after your last exposure to the potentially contaminated water. (In 2011 we identified 15 cases in 6 months)
Schistosomiasis is a disease caused by blood flukes acquired when wading or swimming in infested fresh water lakes and streams. When you are in the water, microscopic parasites burrow through your skin and migrate through your body until they come to their final destination in the veins of the bowel or bladder. Light infections may pass unnoticed but more severe infections may cause blood in the urine or faeces, together with other symptoms
Insect Bites
Mosquitoes, certain types of flies, ticks and bugs can transmit many different diseases. e.g. malaria, dengue fever, yellow fever. Some bite at night, but some during daytime. The main way to avoid illness is to avoid being bitten, so where possible:
If your room is not air conditioned, but screened, close shutters early evening and spray room with knockdown insecticide spray. In malaria regions, if camping, or sleeping in unprotected accommodation, always sleep under a mosquito net (impregnated with permethrin). Avoid camping near areas of stagnant water, these are common breeding areas for mosquitoes etc
Electric insecticide vaporisers are very effective as long as there are no power failures! Electric buzzers, garlic and vitamin B are not effective
Cover up skin as much as possible if going out at night, (mosquitoes that transmit malaria bite from dusk until dawn). Wear light coloured clothes, long sleeves, trousers or long skirts
Use insect repellents on exposed skin. (Choose those containing DEET or eucalyptus oil base. A content of approximately 35% DEET is recommended for tropical destinations.) Clothes can be sprayed with repellents too. Impregnated wrist and ankle bands are also available. Check suitability for children on the individual products
Report any unexplained illness with symptoms such as fever, headache, malaise, muscle aches and fatigue
Malaria
Malaria is probably the most common and most serious disease you will be exposed to when travelling. Malaria is caused by a microscopic parasite transmitted by female mosquitoes when they take a blood meal at your expense. There are four species of malaria parasite, of which Plasmodium falciparum is the most dangerous and can lead to cerebral malaria and death
Malaria usually starts as a fever and you will feel very unwell. Other symptoms may include diarrhoea, headache or a cough. In a malaria area, all illnesses with fever should be considered to be malaria until proved otherwise. Seek medical help as soon as you can if you become ill
Check carefully the areas you plan to travel to and take anti-malarial tablets (prophylaxis) if advised by the travel-health nurse or doctor. Some tablets can be bought over the counter in a chemist but others are only available on prescription. Do not take over-the-counter tablets if prescription-only prophylaxis has been advised
You can get malaria even when taking prophylaxis, but this happens more commonly in individuals who forget to take one or more tablets. It is essential that you take the tablets you are prescribed regularly and on time and for the whole of the recommended time after leaving a malaria area (sometimes for 4 weeks after)
Mosquitoes that transmit malaria bite mainly at night, but this can be any time from dusk onwards and even just after dawn. Use insect repellent containing at least 35% DEET, wear long, loose clothing when possible and consider taking a mosquito net impregnated with permethrin to sleep and rest under. These can be bought in outdoor/camping shops. Do not rely on insect repellent and mosquito nets alone if you have been advised to take prophylaxis as well; all forms of protection are important
Take adequate supplies of the antimalarial agent suited to your area of travel and remember to take it. People die every year from malaria in the UK
Even with the best prophylaxis you may still catch malaria so have a high index of suspicion
Report any unexplained illness with symptoms such as fever, headache, malaise, muscle aches and fatigue
Malaria can occur up to two years after being bitten by an infected mosquito
If you become unwell with fever up to a year after returning from a malaria area, see your GP and tell them you have travelled abroad
View the Malaria Prophylaxis page which contains prices and sources for all anti-malarial medicines
Sun Sense
Sunburn and heat-stroke cause serious problems in travellers. Both are preventable – to avoid, use the following precautionary guidelines:
Increase sun exposure gradually, 20 minutes limit initially
Use sun blocks of adequate Sun Protection Factor strength (SPF 15 minimum). Reapply often and always after swimming and washing. Read manufacturer’s instructions
Wear protective clothing – sun hats etc
Avoid going out between 11am – 3pm, when the sun’s rays are strongest
Take special care of CHILDREN and those with pale skin/red hair
Drink extra fluids in a hot climate
Be aware that alcohol can make you dehydrated
Why factor 15?
The reason experts recommend factor 15, is that this represents the best balance between protection and price. You will get over 90 per cent protection from UVB rays with SPF 15. But no sunscreen, no matter how high the factor, can offer 100 per cent protection
Factor 15 sunscreen offers about 93% protection
Factor 30 sunscreen offers about 96% protection
Factor 60 sunscreen offers about 98% protection
www.cancerresearchuk.org/sunsmart/staysafe/sunscreen/
When Buying sunscreen:
Choose one with an SPF of 15 or above – this will give you over 90% protection
Make sure it is labeled ‘broad spectrum’ – to protect against UVA and UVB
Choose water resistant – it is less likely to wash or be sweated off
Check the ‘use by’ date – most sunscreens have a shelf life of 2-3 years
You don’t have to pay for expensive brands. All types are tested and the cheaper brands are just as effective if used properly – just remember factor 15+
Tips for using sunscreen properly:
Try to apply it 15-30 minutes before going out in the sun
Apply to clean, dry skin and rub in only lightly
Use generous amounts
Re-apply once outside to ensure even coverage
Then re-apply according to manufacturers instructions or more frequently if washed, rubbed or sweated off
Put on before make-up, moisturiser, insect repellant, and so on
Never use it to spend longer in the sun – this will put you at risk of sun damage that could lead to skin cancer
In hotter climates and hotter days in the UK avoid direct sun exposure between 11am and 3pm
Take special care of children and those with pale skin / red hair
Use SPF 60 on any areas of recent scarring / skin damage
You can get severe sunburn in the UK
Do not store sunscreens in very hot places as extreme heat can ruin their protective chemicals
Travel at High Altitude
Medex offer a comprehensive booklet on travelling at high altitude which you can download.
When you return
Have you been travelling to tropical or sub-tropical countries over the summer?
Please maintain a high degree of suspicion of Malaria if you develop any flu-like illness (characterised by fever, headache, joint aches, etc)
If you have been travelling and have returned feeling unwell, especially with an unexplained fever or prolonged diarrhoea you should make an appointment with a doctor
Travel occasionally brings some negative experiences. Please seek support for any unresolved issues from whomever you feel most comfortable with: friends/family/doctor or counselling services
Medical Electives
Medical Indemnity
Contact MPS or MDU and arrange an elective study indemnity policy
Psychological Support
On your elective you may have many new and sometimes distressing experiences including helplessness and frustration witnessing preventable deaths. You may experience significant culture shock and have difficulty adjusting on your return to the UK. It is important to prepare for this and also to ask for help from peers, colleagues, counselling services or your doctor if needed
HIV PEP (Post exposure prophylaxis)
If you think you will need HIV-PEP on your elective please contact Occupational Health at St James’ University Hospital
Travel Health Useful Links
The following links to web sites are for your interest and assistance, however LSMP personnel may not be familiar with all the content of these sites and we may not agree with or endorse the views contained within them
Centre for Infectious diseases – Travellers’ Health
Health Protection Unit Malaria
MASTA – Medical Advice Centres for Travellers Abroad
MEDEX – Medical expeditions
NATHNAC – National Travel Health Network and Centre
NOMAD – Online travel shop including sterile medical kits
Objective Travel Safety Training
PADI – Scuba diving
The British Mountaineering Council
HIV PrEP
These clinics are run in conjunction with Leeds Sexual Health Service (LSH), from the LSMP premises. You will be registered […]
New Start Recovery – Drug & Alcohol Rehab in Leeds
Helping you take back control of your life via inpatient rehab treatment.
Find a Local Service
Select from the dropdown list and then enter your postcode to search for Services in your local area (within 20km).
Health A-Z
Health A to Z Your complete guide to conditions, symptoms and treatments, including what to do and when to get help.
Live Well
Live Well advice about healthy living, including eating a balanced diet, healthy weight, exercise, quitting smoking and drinking less alcohol.
Medicines A-Z
Find out how your medicine works, how and when to take it, possible side effects and answers to your common […]
Talking Saves Lives
18 people die by suicide every day in England and Wales, but help is out there. There’s always someone to […]
Video Library: Health and Care Videos
Health information at your fingertips.
Who Do I See?
Who is the best Healthcare Professional to see for the following conditions: